Atrial fibrillation (AF) is one of the most common and most dangerous cardiac arrhythmias worldwide. Its greatest threat lies in its silence. Many patients live with AF for months or even years without noticeable symptoms, until the condition suddenly manifests as a stroke or severe cardiovascular complication.
Traditional diagnostics rely on episodic monitoring, symptom reporting, or incidental findings. As a result, intervention often comes too late.
A new AI-driven approach, Find-AF, is changing this trajectory by shifting cardiology from reactive diagnosis to predictive prevention. Developed by researchers at the University of Leeds in collaboration with Leeds Teaching Hospitals NHS Trust, Find-AF demonstrates how artificial intelligence, large-scale data analysis, and modern medical system design can identify AF risk up to six months before symptoms appear.
This development is not only a breakthrough in clinical decision support, but it is a glimpse into how predictive intelligence will shape the next generation of medical technologies, including how we approach Medical Device Hardware Design and Electronic Product Design Services in connected healthcare ecosystems.
From Detection to Prediction: A Paradigm Shift in Cardiac Care
For decades, cardiology has focused on detecting abnormalities once they become measurable or symptomatic. Find-AF challenges this model.
By analyzing de-identified health records from over 2.1 million patients, the system uses machine learning to identify patterns that precede atrial fibrillation patterns often invisible to clinicians using traditional tools. The model has since been tested on datasets covering more than 10 million individuals worldwide, highlighting its potential scalability.
This shift from diagnosing disease to predicting risk marks a fundamental transformation in healthcare delivery. It enables early intervention strategies that could prevent strokes, reduce hospital admissions, and significantly improve patient outcomes.
How Find-AF Works: Intelligence Built on Multimodal Data
Multimodal Data Processing
At the core of Find-AF is its ability to process diverse data sources simultaneously. The AI model extracts signals from:
- Electronic health records (EHRs)
- Laboratory test results
- ECG and cardiac rhythm data
- Demographic and clinical history
This multimodal approach allows the system to build a more holistic picture of cardiovascular risk than any single diagnostic test could provide.
For medical technology developers, this reinforces a key principle: modern healthcare solutions are no longer isolated devices. They are systems integrating hardware, software, data pipelines, and clinical workflows.
Pattern Recognition Through Neural Networks
Using deep learning models, Find-AF identifies subtle correlations across patient histories that indicate elevated AF risk. These patterns may include minor irregularities in heart rhythm, lab trends, or combinations of risk factors that would not trigger alarms in conventional screening.
This capability demonstrates the power of neural networks in uncovering latent clinical signals and highlights the importance of designing medical platforms capable of supporting advanced analytics at scale.
Global Scalability Through Federated Learning
One of the most critical innovations behind Find-AF is its use of federated learning. Instead of centralizing sensitive patient data, the model learns from distributed datasets across institutions while keeping data localized and private.
This approach improves accuracy while preserving compliance with data protection regulations, an increasingly important requirement for AI-enabled medical technologies.
The Clinical Impact: Why Predictive AF Detection Matters
Preemptive Stroke Prevention
AF is a leading cause of stroke, yet many strokes occur in patients who are unaware they have AF. Predictive identification enables targeted monitoring, anticoagulation therapy, or lifestyle interventions before catastrophic events occur.
The result is not just an earlier diagnosis but potentially lives saved.
AI-assisted Clinical Decision Support
Find-AF does not replace clinicians; it augments them. By flagging high-risk patients early, the system helps healthcare providers prioritize care and allocate resources more effectively.
This type of decision support will increasingly be embedded into diagnostic platforms, wearables, implantable devices, and hospital systems, reshaping how clinicians interact with technology.
Adaptive Learning for Evolving Risks
As more real-world data is incorporated, the model continues to learn and refine its predictions. This adaptive capability ensures that risk assessment remains relevant across populations, demographics, and changing healthcare practices.
Implications for Medical Device Hardware Design
While Find-AF itself is primarily a data-driven system, its success has far-reaching implications for Medical Device Hardware Design.
Predictive algorithms like Find-AF require devices that can:
- Capture high-quality physiological data continuously
- Operate reliably over long periods
- Integrate securely with digital health platforms
- Support updates as models evolve
This drives demand for next-generation medical hardware that is:
- More intelligent at the edge
- Capable of real-time data processing
- Designed for interoperability
- Built with security and compliance in mind
Wearable ECG monitors, implantable rhythm sensors, and connected diagnostic tools must be designed not just to record data, but to support predictive intelligence throughout their lifecycle.
The Role of Electronic Product Design Services in Predictive Healthcare
Delivering predictive healthcare solutions requires more than algorithms. It requires robust Electronic Product Design Services that bridge the gap between data science and real-world clinical deployment.
Key design considerations include:
- Sensor accuracy and signal integrity
- Power efficiency for continuous monitoring
- Secure data transmission and storage
- Compatibility with healthcare IT standards
- Upgradability to support evolving AI models
Electronic product design teams must collaborate closely with clinicians, data scientists, and regulatory experts to ensure that devices are not only innovative but also safe, compliant, and usable in everyday care settings.
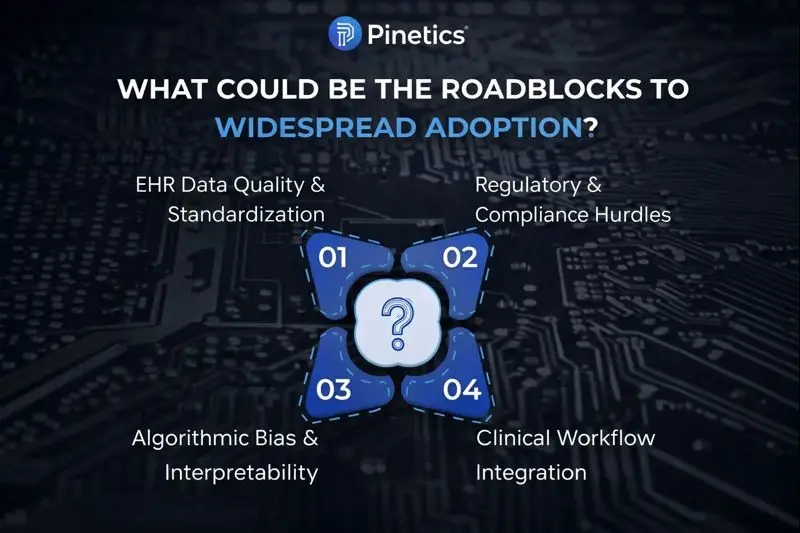
Roadblocks to Widespread Adoption
Despite its promise, predictive AI in cardiology faces several challenges that must be addressed before widespread deployment.
Data Quality and Standardization
EHR systems vary significantly across institutions. Inconsistent data formats, missing fields, and varying clinical practices can impact AI performance. Standardization efforts are essential to ensure reliable predictions on scale.
Regulatory and Compliance Hurdles
AI-driven healthcare solutions must comply with regulations such as HIPAA, GDPR, and MHRA guidelines. Ensuring patient privacy, data security, and clinical validation is non-negotiable.
For device developers, this means embedding compliance considerations directly into hardware and software design, not treating them as afterthoughts.
Algorithmic Bias and Interpretability
Predictive models must be transparent and explainable. Clinicians need to understand why a patient is flagged at high risk, and systems must be monitored to prevent bias across populations.
This places additional responsibility for both AI developers and medical device designers to ensure fairness and accountability.
Clinical Workflow Integration
Even the most advanced AI system will fail if it disrupts clinical workflows. Seamless integration using standards such as FHIR, combined with clinician training and change management, is critical for adoption.
A Glimpse into the Future of Predictive Healthcare
Find-AF represents more than a single innovation; it signals a broader shift in healthcare technology.
In the coming years, we can expect:
- Predictive models embedded directly into medical devices
- Continuous risk assessment replacing episodic screening
- Closer integration between hardware, software, and AI
- healthcare systems that intervene earlier and more precisely
The most impactful medical technologies will not just detect disease; they will anticipate it.
Final Thoughts
Predictive cardiology is redefining how we think about diagnosis, prevention, and patient care. Innovations like Find-AF demonstrate the power of AI to uncover hidden risks and enable earlier, more effective intervention. But realizing this potential requires more than advanced algorithms; it demands thoughtfully engineered medical systems.
At Pinetics, we support this transformation through deep expertise in Medical Device Hardware Design and Electronic Product Design Services. We partner with healthcare innovators to build intelligent, compliant, and scalable medical technologies that integrate seamlessly into modern clinical ecosystems.
As predictive healthcare continues to evolve, the intersection of AI, device engineering, and system design will define the next era of medicine. Pinetics is committed to helping shape that future responsibly, intelligently, and with patient impact at the core.
How do you see AI shaping the future of predictive healthcare?
 Sr. Test Engineer
Sr. Test Engineer Sales Marketing Manager
Sales Marketing Manager Marketing & Sales – BBA : Fresher
Marketing & Sales – BBA : Fresher