When people talk about innovation in healthcare technology, conversation often centers around smarter algorithms, faster processing, or more powerful analytics. But one of the most transformative shifts happening in medicine today is not about speed or power at all.
It is about size.
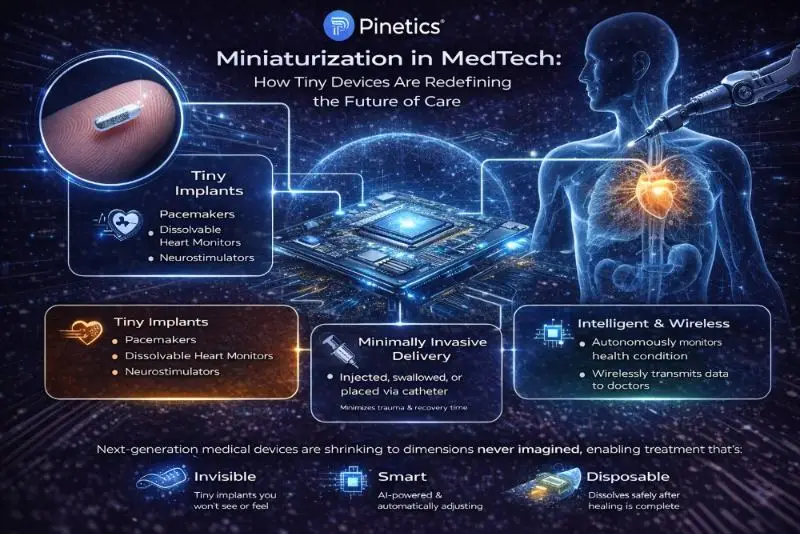
Across the world, researchers and engineers are shrinking life-saving devices to scale once considered impossible. We are entering an era in which medical technology is not only more intelligent but also dramatically smaller, more biocompatible, and seamlessly integrated within the human body.
A powerful example of this transformation emerged from Northwestern University, where researchers recently introduced a groundbreaking technology: a dissolvable pacemaker smaller than a grain of rice, designed specifically for newborns with critical heart conditions.
This innovation is not just a scientific milestone; it represents a complete rethinking of Medical Device Hardware Design, shifting from invasive, permanent implants toward temporary, bioresorbable, intelligent devices that support healing and then simply disappear.
A Pacemaker That Heals the Heart and Then Disappears
For decades, pediatric pacemaker treatment followed the same core paradigm:
- Implant device surgically
- Tether it with leads and wires
- Perform another surgery later for removal or replacement
For fragile newborns, this process carries a particularly high risk. Multiple surgeries are taxing; recovery periods are long, and surgical complications can be life-threatening.
The dissolvable pacemaker changes the equation entirely.
This next-generation device:
- Is injectable using a syringe
- Requires no wires or external leads
- Is activated using a soft, light-responsive external patch
- Supports and stabilizes cardiac rhythm
- Dissolves naturally once its work is complete
No extraction procedure. No permanent implant left behind. Minimal trauma to tiny patients.
This is not just an incremental improvement; it is a fundamental redesign of how we think about therapeutic devices.
The Rise of Invisible Medicine
Historically, medical implants were:
- Large
- Mechanical
- Physically intrusive
- Dependent on batteries and metal structures
Today, material science, wireless energy transfer, and AI-driven sensing are rewriting these design constraints.
We are now developing systems that are:
- Bioresorbable — safely dissolving inside the body after use
- Wirelessly powered — eliminating bulky batteries
- Soft and flexible — able to conform to natural tissue movement
- Intelligent — capable of sensing, adapting, and optimizing function in real time
This new trajectory in Medical Device Hardware Design enables devices that do not just coexist with the human body; they collaborate with it.
Miniaturized devices can:
- Navigate the body’s smallest anatomical pathways
- Deliver highly targeted therapy
- Perform localized monitoring
- Disappear after their job is done
Instead of large surgical implants, treatment becomes quiet, hidden, and personalized.
AI as the Nervous System of Next-Generation Implants
Miniaturization alone is powerful, but when combined with artificial intelligence, it becomes revolutionary.
AI-enabled implantable can:
- Analyze physiological data continuously
- Detect abnormalities in real time
- Autonomously adjust therapy delivery
- Learn from individual patient responses
Imagine devices that:
- Increase pacing only when the heart shows stress signals.
- Adjust insulin release instantly based on metabolic patterns.
- Deliver neural stimulation when early tremor signatures are detected
- Modulate pain management based on real-time biomarkers
Healthcare moves from reactive to predictive and adaptive.
This creates a new category of medical technologies: living systems within living systems.
Rethinking Medical Device Hardware Design from the Ground Up
The shift toward ultra-small, intelligent systems is forcing the industry to revisit every principle of Medical Device Hardware Design.
Engineers are now solving questions such as:
- How do you embed intelligence into devices as small as dust particles?
- How do you power devices without traditional batteries?
- How do systems dissolve safely without leaving traces behind?
- How do circuits behave when made from biodegradable materials?
- How do you maintain function while drastically reducing size?
- How do you build RF communication into a dissolving substrate?
The answers involve multiple converging fields:
- Soft bioelectronics
- Flexible polymers
- Bioresorbable metals
- Micro-scale antennas
- Low-power semiconductor design
- Advanced sensing systems
The future of device design lies at the intersection of:
- Biology
- Materials science
- Electronics
- AI
- Clinical engineering
This interdisciplinary approach is reshaping what “hardware” means in medicine.
From Surgery to Syringe: The New Era of Minimally Invasive Care
Traditionally, minimally invasive meant:
- Smaller incisions
- Laparoscopic entry points
- Robotic precision
Tomorrow’s definition goes further.
Minimally invasive will mean:
- Devices delivered by syringe instead of surgery
- Systems operating silently and automatically
- Implants that self-eliminate once mission-complete
Instead of hardware being something added to the body, it becomes part of the body’s healing process, integrating, performing, and disappearing without disruption.
The goal is not simply to reduce pain or scarring. It is about:
- Lowering infection risk
- Reducing anesthesia exposure
- Eliminating device removal surgeries
- Minimizing hospital stays
- Improving long-term outcomes for vulnerable patients
For infants, elderly patients, oncology patients, and cardiac-compromised individuals, this shift is life-changing.
From Devices You See to Devices You Never Notice
The future of MedTech will be defined by technologies that:
- You cannot see
- You cannot feel
- You may not even realize they are there.
And yet, they will:
- Monitor organs
- Regulate body rhythms
- Communicate wirelessly with clinicians
- Dissolve without intervention
- Support long-term disease management
Medicine is becoming:
- Quieter
- Smaller
- More intelligent
- More deeply integrated
- More human-centric
The most powerful medical technologies of the next decade may not resemble machines at all. They may be fibers, particles, films, or micrometer-scale circuits residing harmoniously within living tissue.
Final Thoughts
Miniaturization is not just an engineering trend; it is a redefinition of how medicine interacts with the human body. Breakthrough innovations such as Northwestern University’s dissolvable newborn pacemaker signal a future where therapy is precise, autonomous, wireless, soft, and ultimately temporary when it needs to be.
We are moving toward a world where devices are designed to serve, heal, and then disappear.
At Pinetics, we play an active role in supporting this transformation. Through advanced expertise in Medical Device Hardware Design, we collaborate with innovators developing next-generation implants, wearables, and connected healthcare technologies. Our focus is on engineering systems that are smaller, safer, smarter, and more biologically aligned, enabling a future where life-saving technology is almost invisible, yet profoundly impactful.
If your organization is shaping the future of MedTech and needs a partner in designing intelligent medical hardware, Pinetics is ready to collaborate with you.
 Sr. Test Engineer
Sr. Test Engineer Sales Marketing Manager
Sales Marketing Manager Marketing & Sales – BBA : Fresher
Marketing & Sales – BBA : Fresher